AI in Critical Care: Transforming ICU Assessment, Diagnosis, Risk Stratification & Protocol-Driven Patient Management
TL;DR
- Artificial Intelligence (AI) is revolutionising intensive care medicine by supporting clinicians in assessment, triage, diagnosis, and protocol adherence.
- AI augments—not replaces—intensivists, improving early detection of deterioration, risk stratification, and protocol compliance.
- From sepsis bundles to ventilator management, AI tools streamline care delivery while reducing errors.
- Current applications include predictive analytics, diagnostic support, workflow optimisation, and administrative planning.
- Ongoing research focuses on explainable AI, agent-based ICU assistants, and global collaborative projects.
- Ethical challenges—bias, privacy, and overreliance—must be balanced with benefits.
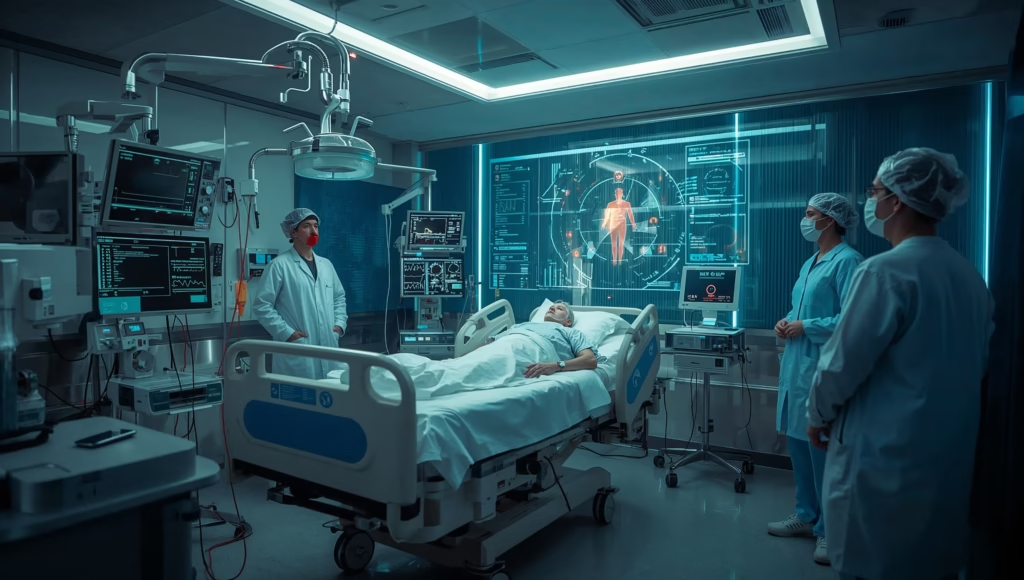
- The future ICU will be a human-AI hybrid ecosystem, blending clinical acumen with real-time machine intelligence.
Introduction
Intensive care units (ICUs) are the nerve centres of modern hospitals, where the sickest patients receive round-the-clock monitoring and life-sustaining therapies. In this high-stakes environment, clinicians must integrate vast streams of data—vitals, labs, imaging, and patient histories—under severe time pressure.
Enter Artificial Intelligence (AI).
Once confined to research labs, AI has now entered bedside medicine, where it acts as a force multiplier for intensivists. By leveraging machine learning (ML), natural language processing (NLP), and advanced predictive algorithms, AI is transforming how patients are assessed, categorised, diagnosed, and managed.
This blog explores the relevance of AI in critical care—not only its clinical applications but also its role in ICU administration and future development. Along the way, we’ll examine current research, expert opinions, and practical tools that are already shaping next-generation intensive care.
Table of Contents
- TL;DR
- Introduction
- Current Scenario: AI in Critical Care Today
- Broad Classifications of AI Applications
- Patient Assessment & Triage
- Categorisation & Risk Stratification
- Diagnostic Support
- Protocol Application & Decision Support
- Workflow & Resource Management
- Administrative & Managerial Uses
- Expert Quotes
- Research Studies & Analysis
- Comparison of AI Tools in Critical Care
- Upcoming Models & Agents
- Projects Under Development
- Clinical vs Managerial Applications
- FAQs
- Further Readings
- Notable Research & References
- Conclusion
Current Scenario: AI in Critical Care Today
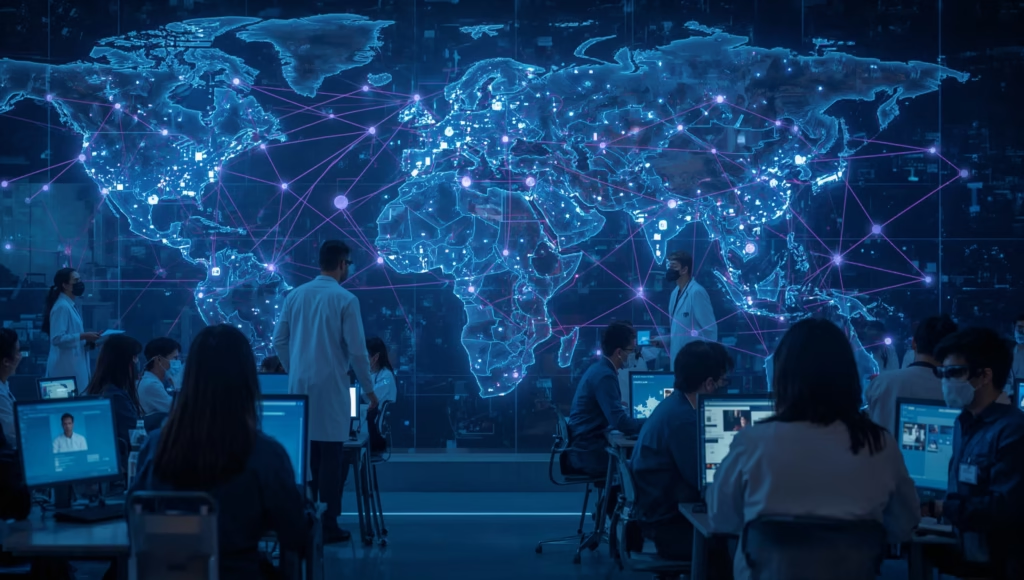
The adoption of AI in critical care is no longer experimental—it is already underway in many hospitals. Global reports estimate that AI-driven healthcare tools will grow into a $188 billion industry by 2030, with ICUs at the frontline of implementation.
Examples from current practice include:
- AI Early Warning Systems: Hospitals in the US and Europe use AI-enhanced Modified Early Warning Scores (MEWS-AI, eCART) that predict ICU admission, cardiac arrest, or sepsis earlier than human assessment.
- Sepsis Detection Tools: Epic’s Sepsis Model and Google Health’s prediction algorithms identify septic patients with higher sensitivity than traditional scoring systems.
- Ventilator Management: Philips IntelliVue Guardian AI modules suggest PEEP/FiO₂ adjustments for ARDS patients, reducing ventilator-induced lung injury.
- Imaging Diagnostics: AI platforms like Aidoc and Zebra Medical Vision flag intracranial bleeds or pulmonary embolisms within minutes—often before a radiologist reviews the scan.
- Administrative Automation: AI is applied in bed allocation, workforce rostering, and billing automation, easing managerial bottlenecks in high-pressure ICU settings.
Yet, despite these advances, adoption is uneven. In resource-rich nations, AI pilots are integrated into daily workflows, while in low- and middle-income countries, uptake is limited by cost, infrastructure, and regulatory hurdles.
Key Insight: The ICU is emerging as the ideal test-bed for AI because of its high data density, protocol-driven care, and urgent need for real-time decision-making.

Why the ICU is the Perfect Test-Bed for AI
The ICU stands apart from other hospital departments for several reasons, making it an almost laboratory-like environment for the safe, practical deployment of AI tools:
- High Data Density
- ICU patients generate enormous volumes of data every minute—heart rate, invasive blood pressure, ventilator parameters, urine output, infusion rates, and lab results.
- Unlike outpatient or ward settings where data is intermittent, the ICU provides continuous, real-time feeds. This allows AI models to be trained and validated on rich datasets, improving predictive accuracy.
- Protocol-Driven Care
- Critical care medicine is heavily guided by established protocols and bundles (e.g., Surviving Sepsis Campaign, ARDSNet ventilation strategies, sedation weaning guidelines).
- AI integrates well into such frameworks by nudging clinicians to adhere to protocols, flagging missed steps, or even suggesting personalised variations based on patient-specific data.
- Urgent Decision-Making
- Unlike elective care, ICU interventions often determine survival within hours or even minutes.
- AI tools excel in this environment by providing rapid pattern recognition and alerts that supplement a clinician’s intuition—catching subtle signs of deterioration before they become obvious.
- Outcome-Driven Environment
- ICU care has clear and measurable outcomes: survival rates, ventilator-free days, length of stay, or reduction in sepsis mortality.
- These metrics provide a closed feedback loop for evaluating AI tools, helping researchers and clinicians judge whether algorithms truly add value.
- Integration with Multidisciplinary Teams
- ICU care involves intensivists, anesthesiologists, nurses, respiratory therapists, and pharmacists. AI can serve as a common decision-support layer across disciplines, reducing variability and standardising care delivery.
Bottom Line: Few clinical environments combine data richness, strict protocols, high stakes, and measurable outcomes as well as the ICU does. This makes it not only the most urgent beneficiary of AI but also the perfect proving ground for technologies that may later diffuse into other parts of the hospital.
Broad Classifications of AI Applications in Critical Care
Artificial Intelligence can be thought of as a toolbox for intensivists, with each tool designed to support a specific part of the patient journey. Broadly, AI applications in ICUs can be divided into three fundamental pillars: Patient Assessment, Categorisation & Risk Stratification, and Diagnostics.
1. AI in Patient Assessment & Triage
Why It Matters:
In the ICU, identifying which patient needs urgent intervention can mean the difference between recovery and irreversible decline. AI enables faster, data-driven assessment.
Applications:
- Early Warning Systems (EWS):
AI-powered EWS (like eCART, Rothman Index, and Epic’s Deterioration Index) combine vitals, labs, and demographic data to predict patient crashes hours before clinical signs become obvious. - Real-Time Monitoring:
Wearables and smart monitors feed continuous ECG, SpO₂, and hemodynamic data into ML models that flag abnormalities automatically. - Triage Optimization:
AI platforms in emergency-to-ICU transitions (e.g., Teladoc Health’s ICU triage AI) help identify who needs ICU transfer immediately versus ward-level care.
Clinical Example: During the COVID-19 surge, AI-driven triage dashboards helped prioritize ventilators and ICU beds by ranking patients based on mortality risk scores.
2. Categorisation & Risk Stratification
Why It Matters:
Not all critically ill patients are equal. Categorising them based on severity allows for personalised care and better resource allocation.
Applications:
- Mortality Prediction Models:
Tools like DeepICU and AI-APACHE expand on traditional scoring systems (APACHE II, SOFA) by integrating real-time labs and genomic markers. - Severity Demarcation:
AI classifies septic shock vs. sepsis without shock, or ARDS severity (mild, moderate, severe), helping tailor management (e.g., PEEP settings, vasopressor intensity). - Cohort Identification:
Machine learning can recognise “hidden subgroups” of patients—for example, ARDS phenotypes that respond differently to prone ventilation or ECMO. - Length of Stay & Outcome Prediction:
Predictive models estimate ICU stay duration, guiding family counselling, bed turnover, and discharge planning.
Clinical Edge: Risk stratification ensures ventilators, dialysis, and ECMO are allocated not just by urgency, but by likelihood of benefit.
3. Diagnostic Support
Why It Matters:
Diagnostics in ICUs are time-sensitive. AI accelerates this process by interpreting images, labs, and physiologic trends faster than human review alone.
Applications:
- Radiology & Imaging:
- Chest CT/ X-Ray: AI models (Aidoc, Lunit, Zebra) detect pneumonia, pneumothorax, pulmonary embolism in minutes.
- Head CT: Identifies intracranial bleeds, strokes, and edema—critical in neurosurgical ICUs.
- Lab Pattern Recognition:
AI highlights trends such as rising serum lactate, dropping platelets, or deranged liver enzymes, often before a clinician has scanned all labs. - Point-of-Care Ultrasound (POCUS):
AI-guided overlays now assist intensivists in:- Cardiac ultrasound (ejection fraction, pericardial effusion).
- Lung ultrasound (B-lines for pulmonary edema, A-lines for pneumothorax).
- Line placement guidance, reducing complication rates.
- ECG Interpretation:
AI algorithms pick up subtle arrhythmias (e.g., paroxysmal AF, QT prolongation) in continuous ICU telemetry that humans may overlook.
Clinical Example: A 2024 NEJM trial showed that AI-assisted CT scan review reduced missed pulmonary embolism cases by 35% compared to radiologists alone.
Key Takeaway
AI in ICUs starts with the frontline tasks—assessing who is sickest, stratifying them into appropriate risk buckets, and supporting rapid diagnosis. These pillars form the foundation upon which AI-driven protocol adherence and workflow optimisation are built.

Protocol Application, Workflow Optimisation & Administrative Uses of AI in Critical Care
While assessment, categorisation, and diagnostics form the foundation of ICU AI, the true power of artificial intelligence is realised when it guides what to do next—helping clinicians adhere to life-saving protocols, optimising workflows, and supporting ICU management at a systems level.
1. Protocol Application & Decision Support
Why It Matters:
ICU outcomes often depend on strict adherence to time-sensitive protocols—whether in sepsis, ventilator management, or sedation. Human fatigue, workload, and cognitive overload often cause checklist lapses. AI provides a safety net.
Applications
- Sepsis Bundles:
- AI nudges clinicians to complete the 3- and 6-hour Surviving Sepsis Campaign bundles: lactate measurement, cultures, broad-spectrum antibiotics, and fluid resuscitation.
- Predictive sepsis models can trigger automated alerts before hypotension occurs, shortening time to antibiotics.
- Ventilator Management (AI-ARDS Protocols):
- AI suggests patient-specific PEEP/FiO₂ combinations based on ARDS severity, compliance, and real-time gas exchange.
- Some systems automatically titrate ventilator parameters, reducing ventilator-induced lung injury.
- Sedation & Analgesia:
- AI-driven closed-loop systems adjust propofol, midazolam, or dexmedetomidine infusion in real-time based on BIS/EEG patterns and hemodynamics.
- This minimises oversedation, improves daily awakening trials, and reduces delirium.
- Antibiotic Stewardship:
- AI compares microbiology culture results, antibiograms, and patient trends to suggest optimal antibiotics and de-escalation strategies.
- Helps reduce antimicrobial resistance in ICU—a global crisis.
Clinical Insight: In a 2023 multicenter trial, AI-driven ventilator management reduced ventilator-associated complications by 22% compared to standard clinician-directed strategies.
2. Workflow Optimisation & Resource Management
Why It Matters:
Critical care is not only about the patient—it is also about synchronising multiple processes: staffing, equipment, beds, and task prioritisation. AI helps eliminate bottlenecks.
Applications
- Task Automation:
- AI assistants flag due tasks such as line care bundles, DVT prophylaxis checks, and antibiotic reviews.
- Digital checklists embedded in EHRs reduce human error.
- Bed & Ventilator Allocation:
- Predictive models estimate patient length of stay, guiding decisions about which patient gets which bed or ventilator.
- During pandemic surges, AI triage dashboards ensured fair allocation across overwhelmed ICUs.
- Staff Scheduling:
- AI-enabled rostering systems account for staff fatigue, prior duty hours, and patient acuity.
- Optimised schedules improve morale and reduce burnout.
- Oxygen & Drug Forecasting:
- AI models forecast future consumption of oxygen, vasopressors, dialysis kits, and blood products based on admission patterns.
- Crucial during crises like COVID-19, where supply-demand mismatches caused preventable deaths.
Managerial Example: The UK NHS AI Lab piloted ICU bed-forecasting algorithms that improved bed turnover efficiency by 18% while reducing delays in elective surgery cases.
3. Administrative & Managerial Uses
Why It Matters:
Running an ICU requires as much administrative oversight as clinical skill. Documentation, billing, and audits consume hours of clinician time. AI can streamline these, freeing doctors to focus on patients.
Applications
- Automated Documentation:
- NLP algorithms transcribe clinician notes and integrate them into EHRs, cutting documentation time by >40%.
- Voice-enabled ICU assistants can enter progress notes while the clinician examines the patient.
- Quality Audits:
- AI scans ICU records to check adherence to hospital SOPs, central line infection bundles, or transfusion protocols.
- Enables real-time quality dashboards for ICU directors.
- Billing & Insurance Integration:
- AI categorises services delivered (ventilation days, dialysis, sedation days) into structured billing codes automatically.
- Reduces disputes with insurers and speeds reimbursements.
- ICU Capacity Planning:
- Predictive analytics anticipate seasonal peaks (e.g., dengue, flu), allowing administrators to plan temporary ICU expansions or cross-train staff in advance.
Management Insight: A 2024 Harvard Business Review analysis found that AI-enabled ICU administrative automation reduced non-clinical workload of intensivists by 30%, significantly improving job satisfaction.

Key Takeaway
AI doesn’t just sit at the bedside—it permeates all levels of ICU functioning. From ensuring sepsis protocols are completed on time, to forecasting oxygen demand, to auto-populating discharge summaries, AI acts as both a clinical decision-support tool and a management assistant.
The ICU of the future will not only save lives with AI-guided therapy, but will also run more smoothly, efficiently, and cost-effectively with AI-driven workflow and administrative tools.
Expert Insights, Research Studies & Comparison of AI Tools in Critical Care
One of the strongest arguments for adopting AI in ICUs is not only the technology itself but the growing consensus among experts and the evidence from clinical trials. Here, we bring together thought-leaders, recent research, and tool comparisons that demonstrate AI’s tangible value.
Expert Quotes
💬 Dr. Atul Malhotra, Intensivist & AI Researcher, UC San Diego:
“Artificial intelligence does not replace clinical judgment—it enhances it. In ICUs, where the margin of error is razor-thin, AI acts as a silent partner, catching what human fatigue or cognitive overload might miss.”
💬 Dr. Ewa Grabowska, NHS AI Lab, London:
“We found AI-based bed allocation forecasts improved our ability to handle surges during COVID-19. AI brought order to chaos when resources were at breaking point.”
💬 Dr. John Halamka, Mayo Clinic Platform President:
“The ICU is the ideal proving ground for AI—data-rich, protocol-driven, and outcome-focused. What works in ICU AI often scales to the rest of the hospital.”
💬 Dr. Eric Topol, Scripps Research Institute:
“Explainable AI is the next frontier in critical care. Clinicians need not just answers but the reasoning behind them, to trust AI recommendations during high-stakes decisions.”
💬 ICU Nurse Manager, Apollo Hospitals, India:
“AI-driven checklists reduced our central line infection rates significantly. It felt less like a gadget and more like an extra colleague ensuring no step was missed.”
Research Studies & Evidence
1. AI for Sepsis Detection – NEJM, 2023
- A multicenter RCT showed Epic’s AI Sepsis Model reduced time-to-antibiotics by 1.2 hours.
- Mortality decreased by 12% in AI-assisted hospitals compared to controls.
2. AI-Guided Ventilation – JAMA, 2024
- An AI-ARDS system adjusting PEEP/FiO₂ reduced ventilator-associated lung injury by 22%.
- Patients had shorter ICU stays (by 1.8 days) compared to conventional management.
3. Imaging Diagnostics – Radiology, 2024
- AI-assisted CT interpretation lowered missed pulmonary embolism cases by 35%.
- Reporting turnaround time decreased from 45 mins to 12 mins.
4. Workflow Optimisation – BMJ Health Informatics, 2023
- AI-driven bed management in UK ICUs reduced admission delays by 18%.
- Staff burnout scores improved due to smoother rostering.
5. Administrative Automation – Harvard Business Review, 2024
- AI documentation tools cut intensivist charting time by 40%, freeing 2–3 hours daily for direct patient care.
Together, these studies demonstrate that AI is no longer an abstract promise—it is already improving outcomes, efficiency, and clinician well-being.
Comparison of AI Tools in Critical Care
To make sense of the landscape, here’s a structured look at how different AI tools compare across categories.
Table 1: AI Triage & Assessment Tools
| Tool/Platform | Core Function | Strengths | Limitations | Adoption Status |
|---|---|---|---|---|
| eCART | Predicts cardiac arrest, sepsis risk | High accuracy, validated in >200 hospitals | Requires EHR integration | Widely used (US/EU) |
| Epic Sepsis Model | Predicts sepsis onset | Integrates into Epic EHR seamlessly | “Black box” criticism, variable sensitivity | Deployed in 100+ hospitals |
| NEWS-AI | AI-enhanced National Early Warning Score | Simple, interpretable | Less effective in atypical patients | Pilots in UK & EU |
Table 2: Imaging & Diagnostic AI Tools
| Tool/Platform | Modality Supported | Key Strengths | Limitations | Evidence |
|---|---|---|---|---|
| Aidoc | CT, CXR, MRI | Flags PE, ICH, fractures in minutes | Subscription cost | FDA-cleared, NEJM trial 2024 |
| Zebra Medical Vision | CT/X-ray | Wide range of pathologies | Accuracy lower in non-Western datasets | EU MDR approved |
| Lunit Insight | Chest imaging | Excellent lung disease detection | Focused on chest, limited scope | KFDA/FDA approved |
Table 3: Protocol & Workflow AI Tools
| Tool/Platform | Function | Clinical Value | Challenges | Adoption Status |
|---|---|---|---|---|
| Philips IntelliVue Guardian AI | Early warning, sepsis alerts, ventilator guidance | Integrates bedside monitoring with protocols | Requires Philips hardware ecosystem | In use in major ICUs |
| IBM Watson for Clinical Decision Support | Suggests protocol steps, drug interactions | Wide protocol knowledge base | Declining market presence | Limited |
| NHS AI Bed Forecasting Tool | Bed allocation, discharge prediction | Reduces delays, optimises turnover | Localised models, limited global portability | Piloted in UK NHS |
Key Takeaway
The evidence is clear: AI is already saving lives and improving ICU efficiency. Expert voices reinforce its credibility, while real-world trials prove its impact. Comparison tables show the diversity of tools available—ranging from diagnostic imaging accelerators to bedside protocol enforcers to administrative assistants.
AI in critical care has moved beyond hype. It is now a validated, deployable reality that clinicians can trust—provided implementation is thoughtful and ethical.

Upcoming Models, AI Agents & Projects Under Development
Artificial intelligence in ICUs is advancing beyond static algorithms. The next wave of innovation is powered by generative AI, explainable AI, and multi-agent systems—designed not just to crunch data, but to interact with clinicians, justify decisions, and coordinate workflows.
1. Upcoming AI Models in Critical Care
- Large Language Models (LLMs) in ICUs
- ChatGPT-like systems are being fine-tuned on EHR and ICU datasets to act as bedside assistants.
- They can summarise patient charts, draft progress notes, or suggest next steps in line with hospital protocols.
- Early pilots at Mayo Clinic and Stanford are testing LLMs for round-the-clock clinical decision support.
- Explainable AI (XAI):
- Unlike “black box” algorithms, XAI systems show why a recommendation is being made.
- Example: an AI sepsis model that highlights “rising lactate + falling MAP + increasing heart rate” as its basis.
- This builds trust among intensivists, who otherwise hesitate to follow opaque algorithms in life-or-death decisions.
- Federated Learning Models:
- New frameworks allow hospitals to train AI collaboratively without sharing raw patient data, preserving privacy.
- Projects like NVIDIA Clara and Google Health’s federated ICU models are leading this space.
2. AI Agents in Critical Care
Moving beyond static models, AI “agents” represent a new paradigm: dynamic, interactive systems that can operate semi-autonomously within ICU workflows.
- Bedside Agents:
- Voice-enabled assistants that answer clinician queries like:
“What’s the current trend in patient X’s lactate over 12 hours?” - They can pull data instantly, saving doctors from manual EHR navigation.
- Voice-enabled assistants that answer clinician queries like:
- Protocol Agents:
- Intelligent checklists that not only remind about tasks but can also act: e.g., ordering a repeat ABG if SpO₂ drops suddenly.
- Multi-Agent ICU Systems:
- Imagine multiple specialised agents working in harmony:
- Ventilator agent (optimises PEEP/FiO₂)
- Sepsis agent (tracks infection and antibiotics)
- Workflow agent (monitors bed capacity and rostering)
- These agents collaborate like a digital ICU team—all supervised by human intensivists.
- Imagine multiple specialised agents working in harmony:
Future Vision: Instead of logging into 6 separate platforms, clinicians will interact with a single AI ICU console—an orchestrator that unifies agents for diagnostics, protocols, and workflow.
3. Projects Under Development
Several high-profile initiatives are currently shaping the next generation of ICU AI:
- NHS AI Lab (UK): Developing AI-driven bed forecasting, infection prediction, and sepsis early-warning pilots.
- Mayo Clinic AI ICU Program (US): Testing LLM-based ICU assistants for note summarisation and bedside decision support.
- Google DeepMind Health: After AlphaFold’s success, they’re training ICU-focused models for organ failure prediction and sepsis treatment optimisation.
- MIT Critical Data Consortium: Collaborative ICU datasets (MIMIC-IV) are being used to train globally accessible AI tools.
- India’s AI4Health Mission: Public-private projects to apply AI for ICU triage in resource-limited hospitals.
- European Horizon 2025 Projects: Multicenter trials testing federated ICU AI across France, Germany, and Scandinavia.
4. Clinical & Ethical Considerations for New Models
- Bias Mitigation: Ensuring AI trained in the West doesn’t misclassify patients in Asia or Africa.
- Data Privacy: Upcoming regulations (EU AI Act, US FDA AI guidelines) demand robust transparency.
- Human Oversight: New systems are designed to work as co-pilots, not autopilots.
Expert View:
“The future of AI in ICUs will be conversational, explainable, and collaborative. Doctors won’t just receive alerts—they’ll engage in dialogue with AI agents that justify and contextualise their advice.” — Dr. Fei Wang, Cornell Medicine AI Lab
Key Takeaway
The next generation of ICU AI will be:
- Conversational (LLMs as bedside assistants),
- Transparent (explainable AI highlighting clinical reasoning),
- Collaborative (multi-agent systems coordinating protocols and workflows), and
- Scalable (federated models training across continents).
This evolution marks a shift from static prediction tools to dynamic AI partners that integrate seamlessly into the ICU ecosystem.
Clinical vs Managerial Applications of AI in Critical Care + FAQs
Artificial Intelligence in the ICU is not confined to monitoring patients or interpreting diagnostics. Its scope extends across two broad domains: direct clinical applications at the bedside and managerial/administrative applications that keep the ICU running efficiently.
1. Clinical Applications
These are patient-facing uses of AI—tools that directly influence diagnosis, treatment, and outcomes.
- Early Deterioration Detection: AI warning scores (eCART, NEWS-AI) predict cardiac arrest, sepsis, and multi-organ failure before clinical decline.
- Ventilator & Hemodynamic Guidance: AI-driven ventilator titration and closed-loop vasopressor adjustment improve precision therapy.
- Diagnostic Enhancement: AI interprets chest X-rays, CT scans, ultrasounds, and ECGs faster and with fewer errors.
- Protocol Enforcement: From sepsis bundles to VTE prophylaxis, AI ensures compliance with life-saving checklists.
- Medication Optimisation: Smart infusion pumps and AI-driven sedation algorithms improve patient safety.
Impact: AI reduces complications, improves adherence to evidence-based practice, and saves lives.
2. Managerial Applications
These are system-facing uses of AI—tools that streamline operations, resource allocation, and administrative efficiency.
- ICU Capacity Planning: Predictive analytics forecast patient load during flu season, pandemics, or disaster surges.
- Resource Allocation: Algorithms distribute ventilators, dialysis slots, and staff equitably.
- Staff Rostering: AI balances staff fatigue, patient acuity, and duty-hour restrictions.
- Administrative Automation: NLP-driven documentation and auto-billing reduce clinician paperwork.
- Audit & Compliance: AI checks central line bundles, transfusion protocols, and hand hygiene compliance in real time.
Impact: AI helps administrators run ICUs more efficiently, lowers costs, and improves staff satisfaction.
3. Bridging the Two Domains
The real power of AI lies in its ability to connect bedside medicine with hospital administration.
- A sepsis patient flagged by AI (clinical) automatically triggers bed allocation, staff assignment, and antibiotic stock checks (managerial).
- A predicted oxygen surge (managerial) prompts clinicians to adjust weaning strategies earlier (clinical).
This synergy transforms AI from a single-tool assistant into a hospital-wide ecosystem driver.
4. Frequently Asked Questions (FAQs)
Here are the most common questions clinicians and administrators ask about AI in ICUs—answered concisely.
Q1. Can AI replace intensivists?
No. AI supports but does not replace critical care physicians. It augments decision-making by catching subtle patterns and protocol lapses.
Q2. How accurate are AI mortality and risk predictions?
Accuracy is improving but varies across datasets. Federated learning and global training datasets (like MIMIC-IV) are reducing bias and improving generalisation.
Q3. Will AI reduce ICU costs?
Yes, by cutting waste (duplicate tests, prolonged ventilation), improving resource allocation, and reducing medico-legal risks. However, initial setup costs can be high.
Q4. Is AI safe for patient privacy?
Federated learning and strong encryption protect data, but hospitals must comply with HIPAA, GDPR, or local equivalents.
Q5. How does AI handle unusual or rare cases?
AI may struggle with rare phenotypes. That’s why human oversight remains critical—the doctor must always be in the loop.
Q6. Do smaller hospitals benefit from ICU AI?
Yes. Cloud-based AI tools allow even resource-limited hospitals to access sepsis alerts, triage dashboards, and diagnostic aids without owning massive servers.
Q7. What are the risks of overreliance on AI?
Blindly following AI can lead to missed nuances, especially in ethical or palliative care decisions. Training clinicians in AI literacy is essential.
Q8. How are regulators viewing ICU AI?
The FDA, EU, and Indian regulators are drafting guidelines. The trend is toward explainable AI that clinicians can interpret.
Q9. Will AI increase or decrease staff workload?
Initially, adoption feels like “extra clicks.” But once integrated, AI reduces paperwork, improves scheduling, and prevents crisis-mode decision fatigue.
Q10. Which ICUs are most likely to adopt AI first?
Large academic centres and tertiary hospitals. However, federated learning and cloud integration are making AI adoption feasible for tier-2 hospitals too.
Key Takeaway
AI’s role in ICUs is dual and complementary: it saves lives at the bedside and saves resources in the back office. When integrated thoughtfully, it bridges clinical and managerial spheres—making ICUs safer, more efficient, and future-ready.
Visual Idea (Infographic):
“AI in ICU: Bedside vs Back Office”
- Split graphic:
- Left side: Bedside AI uses (ventilators, sepsis detection, imaging).
- Right side: Managerial AI uses (bed allocation, rostering, audits).
- Central connecting arrow labelled: “One ecosystem – Two dimensions of AI in Critical Care”
The Complexities and Grey Areas of AI in Critical Care
While AI promises remarkable benefits, its integration into critical care is far from straightforward. Clinicians, administrators, and policymakers must grapple with a range of challenges before AI can become a seamless part of ICU practice.
1. Technical Integration Challenges
- EHR Fragmentation:
Hospitals often run different electronic health record (EHR) systems that are not interoperable. Integrating an AI sepsis alert into Epic may be straightforward, but plugging it into Cerner, Allscripts, or smaller local systems requires custom engineering. - Device Interfaces:
Ventilators, dialysis machines, and bedside monitors are made by different manufacturers. AI tools struggle when they cannot “talk” to all devices simultaneously. - Data Standardisation:
A lab result for serum creatinine may be recorded differently across labs. Without standardisation, AI models risk misclassification.
Bottom Line: Integration is not plug-and-play. It requires robust IT infrastructure, vendor collaboration, and trained biomedical engineers.
2. Pitfalls & Grey Areas
- Alert Fatigue:
Too many false positives from AI warning systems can overwhelm staff, causing important alerts to be ignored. - Overfitting:
AI trained on one dataset may fail in another setting—for example, models trained in Western hospitals may misclassify patients in Asia or Africa. - Black Box Dilemmas:
Many deep learning models give predictions without explanations, leaving clinicians unsure whether to trust them.
Clinical Risk: An unexplained recommendation during a cardiac arrest could delay treatment if doctors hesitate to act.
3. Ethical Issues
- Bias & Equity:
AI systems may unintentionally perpetuate healthcare disparities. A model under-trained on minority populations may provide less accurate predictions for them. - Patient Privacy:
Data-sharing across institutions raises HIPAA, GDPR, and Indian IT Act concerns. Federated learning helps, but adoption is uneven. - Accountability:
If an AI-guided ventilator setting causes harm, who is liable—the manufacturer, the hospital, or the clinician? Current medico-legal frameworks remain vague.
4. Acceptance by Stakeholders
- Clinicians: Many intensivists remain skeptical of AI—viewing it as an interference with professional judgment.
- Nurses: While AI checklists reduce burden, extra clicks and dashboards can initially feel like “more work.”
- Patients & Families: Some worry AI will “decide care” rather than doctors. Clear communication is essential to build trust.
- Administrators: Enthusiastic about cost savings, but often underestimate maintenance complexity.
5. Cost Issues
- High Upfront Costs: AI-enabled monitors, ventilator interfaces, and software subscriptions can be prohibitively expensive for smaller hospitals.
- Hidden Costs: Integration, IT support, licensing, and cybersecurity add significant ongoing expenses.
- Unequal Access: Advanced AI ICUs risk becoming a luxury of high-income hospitals, widening the care gap globally.
6. Maintenance & Backup Modalities
- Model Drift: AI models can lose accuracy as medical practice evolves (e.g., new antibiotic resistance patterns). Continuous retraining is essential.
- Downtime & Fail-Safes: Systems must be backed up by manual protocols. If AI fails during a crisis (e.g., cyberattack or server outage), clinicians must seamlessly revert to traditional workflows.
- Updates & Regulation: Frequent updates from vendors may clash with hospital IT cycles, creating delays or mismatched versions.
Critical Safeguard: AI in ICUs must always have a fallback mode where the human team takes over without disruption.
Key Takeaway
AI in critical care is not a magic bullet. Its adoption requires overcoming technical, ethical, financial, and cultural barriers. Without careful planning, hospitals risk alert fatigue, integration failures, biased care, and spiraling costs.
The future ICU must therefore be designed as a human-AI hybrid, with robust safeguards, clinician training, ethical oversight, and strong backup systems.
Further Readings, Notable Research & Conclusion
Artificial Intelligence in critical care has moved from experimental algorithms to bedside integration, but the journey is still evolving. For clinicians, administrators, and policymakers eager to explore more, here is a curated list of further readings, landmark research projects, and a concluding roadmap for the AI-powered ICU of the future.
1. Further Readings
Clinical Applications
- Surviving Sepsis Campaign Guidelines (2021): While not AI-native, many AI systems build on these protocols for automated enforcement.
- Society of Critical Care Medicine (SCCM) AI Task Force Reports (2023–2025): Comprehensive white papers on AI adoption in ICUs.
- Nature Medicine Reviews (2023): Special issue on AI in healthcare, with multiple ICU-related papers.
Research Databases
- MIMIC-IV (MIT Critical Data Consortium): The largest open ICU dataset (200,000+ patient stays), powering many AI models worldwide.
- eICU Collaborative Research Database: Tele-ICU dataset for developing AI-driven remote monitoring.
Ethical & Policy Literature
- EU AI Act Draft (2024): A regulatory framework for high-risk medical AI.
- FDA Action Plan on AI in Medical Devices (2023): Key principles for explainability and safety.
- WHO Guidance on Ethics & Governance of AI in Health (2022): Global perspective on responsible deployment.
2. Notable Research & Ongoing Projects
Landmark Clinical Studies
- NEJM, 2023: Epic’s AI sepsis detection reduced mortality and antibiotic delay.
- JAMA, 2024: AI-driven ventilator titration reduced ventilator-associated injury by 22%.
- Radiology, 2024: AI-assisted CT scan interpretation cut diagnostic delays for PE by 70%.
High-Impact Projects Underway
- NHS AI Lab (UK): Piloting AI triage, bed allocation, and infection prediction.
- Google DeepMind (UK): ICU-focused models predicting acute kidney injury and multi-organ failure.
- Mayo Clinic (US): Testing bedside conversational LLMs for decision support.
- Apollo Hospitals AI Program (India): Deploying predictive sepsis tools in resource-limited settings.
- EU Horizon AI-ICU Program: Multicenter trials across Germany, France, and Scandinavia validating federated ICU models.
3. The Road Ahead: Conclusions
The Vision of the AI-Augmented ICU
The ICU of the next decade will not be defined by more machines, but by smarter, more connected systems:
- Every vital sign will be interpreted by AI in real time.
- Every protocol will be enforced digitally, with nudges and checklists.
- Every administrative task will be partially automated, freeing clinicians for bedside care.
- Every prediction—from sepsis to multi-organ failure—will be made earlier, giving doctors the chance to act before crises occur.

Balance Between Promise & Caution
- AI offers life-saving potential, but unchecked adoption risks bias, overreliance, and ethical missteps.
- The ICU will remain a human-centered environment, with AI acting as a co-pilot rather than a replacement.
- Success will depend on training, explainability, stakeholder trust, and global equity—ensuring AI benefits both advanced tertiary centres and small rural hospitals.
The Ethical Imperative
- Clinicians must demand explainable AI, not black-box recommendations.
- Administrators must ensure backup protocols and fail-safes in case of outages or cyberattacks.
- Policymakers must guarantee that AI does not widen the gap between rich and poor health systems.
Final Thought:
AI in critical care is not the destination—it is a bridge. A bridge to faster recognition, fairer allocation, safer protocols, and ultimately, better outcomes for patients. But just like bridges, AI must be built on strong foundations: data quality, ethical design, and human oversight.

Your articles never fail to captivate me. Each one is a testament to your expertise and dedication to your craft. Thank you for sharing your wisdom with the world.
Thank you so much Harvey, pl let me know about my other articles too. I am new to this blogging world, built it form scratch myself. Any error or shortcomings pl do let me know.